Translate this page into:
Hypokalaemic quadriparesis following torsemide and spironolactone use
2 Department of Geriatric Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
3 Department of General Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India
Corresponding Author:
Indrajeet Singh Gambhir
Department of Geriatric Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh
India
iac2k10@gmail.com
| How to cite this article: Kaur U, Chakrabarti SS, Choudhury AK, Gambhir IS. Hypokalaemic quadriparesis following torsemide and spironolactone use. Natl Med J India 2018;31:347-348 |
Abstract
Mild hypokalaemia is a common electrolyte abnormality following therapeutic doses of diuretics such as torsemide. If undiagnosed and untreated, hypokalaemia progresses and smooth muscle, skeletal muscle and the heart are affected. Potassium-sparing diuretics such as spironolactone are commonly added to loop diuretics to prevent symptomatic hypokalaemia. We present a patient with moderate hypokal-aemia associated with the use of torsemide and spironolactone, resulting in quadriparesis, hospitalization and electrophysio-logical abnormalities.
Introduction
Hypokalaemia (serum potassium <3.5 mmol/L) is a common electrolyte abnormality encountered by physicians. Constipation, urinary retention, muscular paralysis and cardiac arrhythmias are the usual manifestations of hypokalaemia. The common causes of hypokalaemia include diarrhoea, vomiting, drugs, hyperaldo-steronism of any aetiology, thyrotoxicosis and renal tubular acidosis.[1] Among drugs, insulin, beta-2-agonists and diuretics are more frequently implicated. Thiazides, loop diuretics and carbonic anhydrase inhibitors—all are known to cause hypokalaemia.[1],[2] It is uncommon for potassium levels to decrease to <3 mmol/L in a patient treated with thiazide/torsemide on an outpatient basis.[2] The risk is further minimized by co-administration of potassium-sparing diuretics such as spironolactone/eplerenone.[2] We present an atypical case of hypokalaemic quadriparesis associated with torsemide and spironolactone use.
The Case
A 53 -year-old man presented with chief complaints of progressive symmetrical weakness of bilateral upper and lower limbs for 7 days. He complained of difficulty in performing daily activities such as walking without support, getting up from a squatting position and making overhead movements of the shoulder such as combing hair but could button up his shirt. There were no features suggestive of sensory loss, cranial nerve involvement, bladder or bowel abnormality, tremors, ataxia, rigidity or dyspnoea. The weakness was neither preceded by vomiting, diarrhoea, starvation or hyperhidrosis nor was triggered by heavy exercise or a high carbohydrate diet. There were no similar episodes in the past in the patient or his family members. There was no history of ingestion of clay. At presentation, the patient had a blood pressure of 94/60 mmHg in the supine position with no significant fall on sitting and standing position, with his other vital signs stable and normal higher mental functions. Sensory and cranial nerve examination were normal. Motor examination showed normal bulk but reduced muscle tone in the upper and lower limbs. Power was also reduced to 4/5 in bilateral upper limbs (shoulder, elbow and wrist) and lower limbs (hip, knee and ankle) for all movements. All deep tendon reflexes were present and bilateral plantars were down-going.
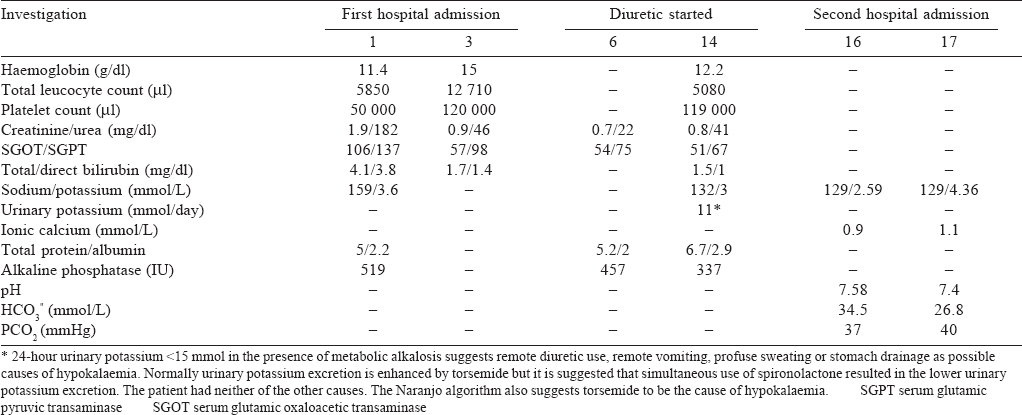
His past history revealed that he had been admitted and treated for malaria, 10 days before the onset of these symptoms, had recovered fully and was discharged. A possibility of chronic liver disease was considered and he was started on a combination of torsemide 10 mg and spironolactone 50 mg daily for oedema, with a plan to investigate further on follow-up. The patient was not on any other medication since discharge. His blood sugar, calcium and phosphate were normal. His HIV status, hepatitis B surface antigen and hepatitis C virus antibody were negative. While other biochemical parameters showed an improving trend by the second visit, the patient had developed mild hypokalaemia. Urinary potassium was low [Table - 1]. Thyroid function was normal, the electrocardiogram showed sinus tachycardia and a Doppler ultrasound of the abdomen did not reveal any abnormality. Cerebrospinal fluid examination was also normal. At this point, a possibility of acute immune demyelinating polyneuropathy was considered and a nerve conduction study (NCS) was done urgently considering the potential for complications. A reduced compound muscle action potential amplitude in bilateral common peroneal nerves and ulnar nerves, absent F waves in bilateral posterior tibial nerves and impersistent F waves in bilateral median nerves were observed. Conduction velocities, distal latencies and sensory nerve action potentials were normal. This was suggestive of acute motor axonal neuropathy but specific treatment was deferred because of the lack of danger signs. By day 3 of admission, the serum potassium decreased further, and an arterial blood gas analysis revealed metabolic alkalosis. Torsemide and spironolactone were discontinued, and the patient was treated with oral potassium supplements. By day 4, he had complete recovery from his symptoms which paralleled the improvement in hypokalaemia and metabolic alkalosis. His blood pressure too corrected with oral fluid supplementation and discontinuation of diuretics. Considering the rapidity of improvement, a diagnosis of hypokalaemic paralysis was made. Acute motor axonal neuropathy is not known to recover in 24 hours and hence was disregarded as a possible diagnosis. After 2 days of observation, the patient was discharged as he had recovered completely.
Discussion
Our patient presented with mild hypokalaemia. His history did not reveal any non-renal causes of hypokalaemia such as vomiting, diarrhoea, starvation or hyperhidrosis nor was hypokalaemia triggered by heavy exercise or a high carbohydrate diet. The absence of a positive family history and prior similar episodes ruled out familial periodic paralysis syndromes. There was no history of ingestion of clay. Anabolic states such as haematopoietic factor supplementation and the use of hormonal drugs such as insulin and beta-agonists were similarly excluded by history. This along with a normal thyroid profile excluded redistributive abnormalities of potassium. Arterial blood gas analysis was not done at admission but only when hypokalaemia worsened to 2.59 mEq/L on day 3 of admission. Metabolic alkalosis was thought to be due to diuretic use as was worsening hypokalaemia. Moreover, this ruled out renal tubular acidosis as a probable cause of hypokalaemia. The patient was worked up for other causes of renal potassium wasting. Salt-wasting nephropathies were excluded from the differentials as serum potassium spontaneously corrected on stopping diuretic medication. Hyperaldosteronism and pseudo-hyperaldosteronism are not known to be associated with a low blood pressure state and also would not have corrected spontaneously by withdrawal of the diuretic. Hypomagnesaemia is known to be an important cause of refractory hypokalaemia. Although the serum magnesium level was not measured, spontaneous correction of hypokalaemia and symptoms makes this an unlikely possibility. We therefore narrowed down on torsemide and spironolactone combination as the most likely aetiology of hypokalaemia in this patient. This was corroborated further by a high Naranjo score.
Among diuretics, loop diuretics, thiazides and acetazolamide are known to cause hypokalaemia.[2] This is related to the dose and duration of the use of diuretic. Potassium-sparing diuretics such as spironolactone and eplerenone are often added to torsemide to prevent the occurrence of hypokalaemia. Hypokalaemia may be preceded or superseded by metabolic alkalosis and ifunmonitored, can manifest as quadriparesis.[1],[2] There are some case reports of diuretic abuse-induced hypokalaemic paralysis,[3],[4] but none with torsemide and spironolactone combination in a therapeutic dose for a short period. Our patient highlights 2 relevant points. First, the risk of hypokalaemic paralysis with torsemide use is not nullified even by concomitant administration of spironolactone. Second, a picture similar to acute motor axonal neuropathy can be seen in NCS in hypokalaemic paralysis. Similar electrophysiological findings have been emphasized in some of the other published reports in which patients with hypokalaemia had a reduction in CMAP and absent F waves.[5] That hypokalaemia is associated with aberrant nerve conduction is expected as potassium is the predominant ion regulating the resting membrane potential of nerves.[6]
On applying the Naranjo scale of adverse drug reaction causality assessment, the association between hypokalaemic paralysis and torsemide/spironolactone was classifiable into ‘probable’ category.[7] Physicians should be vigilant for hypokalaemic quadriparesis even with torsemide and spironolactone combination. The NCS should not be disregarded but can give a confusing picture in hypokalaemic paralysis. A trial of potassium supplementation, therefore, should be given in patients with acute onset pure motor paralysis with hypokalaemia, before exposing them to immunomodulator therapies or plasmapheresis, even in the presence of suggestive findings on NCS.
Conflicts of interest. None declared
| 1. | Palmer BF. A physiologic-based approach to the evaluation of a patient with hypokalemia. Am J Kidney Dis 2010;56:1184-90. [Google Scholar] |
| 2. | Veltri KT, Mason C. Medication-induced hypokalemia. PT 2015;40:185-90. [Google Scholar] |
| 3. | Cawley DT, Curtin PT, McCabe JP. Hypokalaemic paralysis secondary to thiazide diuretic abuse: An unexpected outcome for cauda equina syndrome. Evid Based Spine Care J 2011;2:51-3. [Google Scholar] |
| 4. | Mayr FB, Domanovits H, Laggner AN. Hypokalemic paralysis in a professional bodybuilder. Am J Emerg Med 2012;30:1324.e5-e8. [Google Scholar] |
| 5. | Sharma CM, Nath K, Parekh J. Reversible electrophysiological abnormalities in hypokalemic paralysis: Case report of two cases. Ann Indian Acad Neurol 2014;17: 100-2. [Google Scholar] |
| 6. | Cheng CJ, Kuo E, Huang CL. Extracellular potassium homeostasis: Insights from hypokalemic periodic paralysis. Semin Nephrol 2013;33:237-47. [Google Scholar] |
| 7. | Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981;30: 239-45. [Google Scholar] |
Fulltext Views
1,354
PDF downloads
288




