Translate this page into:
Prevalence of risk factors for non-communicable diseases in a rural tribal population of Mokokchung, Nagaland, India
2 National Institute of Epidemiology (Indian Council of Medical Research), # R-127, 3rd Avenue, Tamil Nadu Housing Board, Chennai 600077, Tamil Nadu, India
Corresponding Author:
Prabhdeep Kaur
National Institute of Epidemiology (Indian Council of Medical Research), # R-127, 3rd Avenue, Tamil Nadu Housing Board, Chennai 600077, Tamil Nadu
India
kprabhdeep@gmail.com
| How to cite this article: Tushi A, Rao SR, Pattabi K, Kaur P. Prevalence of risk factors for non-communicable diseases in a rural tribal population of Mokokchung, Nagaland, India. Natl Med J India 2018;31:11-14 |
Abstract
Background Non-communicable diseases (NCDs) are the leading cause of mortality in India. The northeastern part of India has a high burden of NCDs. However, data on the prevalence of risk factors for NCDs in the rural tribal population of Nagaland are limited. We estimated the prevalence and awareness level of risk factors for NCDs in the rural population of Mokokchung district, Nagaland.Methods In a cross-sectional survey, we selected 472 subjects aged 25–64 years, stratified by age and sex, in 20 villages, using a cluster sampling technique. The WHO STEPS tools were used to collect data on behavioural risk factors, and anthropometric, blood pressure and capillary glucose measurements. The proportion of subjects with each NCD risk factor was determined overall and in various age and sex subgroups.
Results The 472 subjects had a median age of 44.5 years, 92 (19.5%) reported current smoking and 75 (15.9%) reported current alcohol use. Among 236 males, 90 (38.1 %) were current smokers and 65 (27.5%) were current alcohol users, whereas of the 236 females, only 2 (0.8%) and 10 (4.2%) were current smokers and current alcohol users, respectively. The use of smokeless tobacco was common among both males (139/236; 58.9%) and females (117/ 236; 49.6%). Inadequate intake of fruits and vegetables was reported by 189 (80.1%) males and 221 (93.6%) females. Insufficient physical activity was observed only among 16 (3.4%) participants. Prevalence of hypertension and a body mass index of 23.0–27.49 kg/m2 was 43.2% and 32.4%, respectively.
Conclusions We observed a high prevalence of behavioural risk factors for NCDs and of hypertension in rural tribal people in Nagaland. The primary healthcare system needs to be strengthened in this area to improve detection and management of hypertension. Mass and print media campaigns and provision of cessation services may also be helpful.
Introduction
Chronic diseases and injuries were the leading causes of death and disability in India in 2011.[1] The common modifiable risk factors that lead to mortality from non-communicable diseases (NCDs) include high blood pressure, suboptimum blood glucose, low intake of fruits and vegetables, use of tobacco, high blood cholesterol, indoor smoke from solid fuels, physical inactivity, overweight and obesity, and use of alcohol.[1] WHO recommends the use of standard tools for surveillance of risk factors for NCDs to enable comparisons across populations.[2]
The northeastern parts of India have a large population of tribals with distinct lifestyles. The use of tobacco in some form by young people ranged from 48% in Sikkim to 77% in Mizoram; this is above the Indian average of 39%. Alcohol consumption among young men of the northeast was also above the Indian average of 21%.[3] In 2007–08, a survey was done in Mizoram to ascertain the prevalence of risk factors for NCDs using the standard WHO STEPS tools.[4] The survey found a high prevalence of various risk factors. We anticipated a high prevalence of risk factors for NCDs in Nagaland, a neighbouring state, given the cultural similarities. We, therefore, estimated the prevalence of risk factors for NCDs among the rural tribal population of Mokokchung district, Nagaland.
Methods
Study design, setting and participants
We did a cross-sectional survey in Mokokchung district, Nagaland. The study population included all those who were 25–64 years of age. As per the 2011 Census, 91.7% of the population in this district belonged to the scheduled tribes (mostly Ao tribe); further, it had an average literacy rate of 91.6% and 71.4% of the people lived in rural areas.[5]
Sample size and sampling procedure
Assuming a 57% prevalence of tobacco use in Nagaland (GATS 2010),[6] one would need a sample size of 118 to achieve 10% absolute precision for 95% confidence interval (CI), with a design effect of 1.25. We multiplied this calculated sample size by 4 to estimate the prevalence in four strata, i.e. males and females in 25–44 years and 45–64 years age group. Therefore, the calculated total sample size was 472.
We used a cluster sampling method to first select 20 villages (primary sampling units) among 108 villages using probability proportional to size linear systematic sampling (PPSLSS) from the list of villages in the district as per the 2011 Census. In each of the selected villages, a household was randomly selected as the starting point and individuals were surveyed in the contiguous households till the target number of eligible participants was reached. In each household, two individuals, one male and one female were surveyed.
Data collection
An interviewer-administered questionnaire was used to collect data on sociodemographic and behavioural risk factors. Weight was measured to the nearest 0.1 kg using a calibrated electronic weighing scale (Seca Robusta 813; Seca, Hamburg, Germany). Height was measured to the nearest 0.1 cm using calibrated stadiometer (Seca Medical scales; Seca, Hamburg, Germany). Waist circumference was measured to the nearest 0.1 cm at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest. Blood pressure was measured at the right arm after the subject had been sitting for at least 5 minutes using an electronic automatic blood pressure apparatus (Omron HEM-7130; Omron Healthcare India). The average of the two readings taken 5 minutes apart was recorded.
Operational definitions
Current smoker was defined as a person using any smoking tobacco products at the time of the survey.[2] Current smokeless tobacco user was defined as a person using smokeless tobacco products at the time of survey. Current alcohol consumer was defined as consumption of alcohol within the previous 12 months.[2] One serving of fruits or vegetables was considered 80–100 g.[2] We used the WHO definitions for physical activity, briefly inadequate physical activity was defined as physical activity <150 minutes of moderate intensity physical activity or 75 minutes of vigorous-intensity physical activity a week.[7]
Central obesity was defined as waist circumference of ≥90 cm in males and ≥80 cm in females.[8] Obesity and overweight were diagnosed on the basis of modified classification of body mass index (BMI) recommended for Asians.[9]
Hypertension was defined as systolic blood pressure >140 mmHg and/or diastolic blood pressure >90 mmHg, or use of antihypertensive medications.[10]
Data analysis
Proportion of persons with each risk factor and 95% CI were calculated using Epi Info 3.5.4 (from www.cdc.gov/epiinfo/support/downloads/prevversions.html). Prevalence of risk factors was compared across age (25–44 years and 45–64 years) and sex groups.
Human subject protection
The study was approved by the National Institute of Epidemiology ethics committee and each participant gave an informed consent. Patients with newly detected hypertension/diabetes were referred to the closest district hospital for further management.
Results
Sociodemographic characteristics
We surveyed 472 participants between 25 and 64 years of age. Among the 472 participants, 405 (85.8%) had received school level education. The most common occupation was farming (133, 28.2%) followed by a government job (111, 23.5%). The median household income was ₹11 000 (US$ 172) per month.
Behavioural risk factors
Smoking tobacco. Current smoking was reported by 90 (38.1%) males and 2 (0.8%) females. The prevalence was similar in the two age groups among males [Table - 1]. The commonest type of tobacco smoked among current smokers was beedi (84/92 [91.3%]).
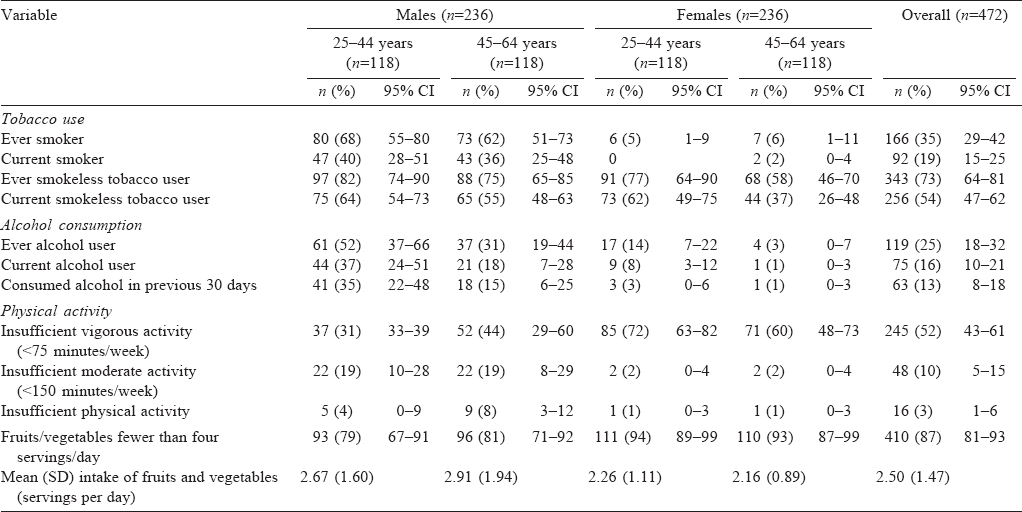
Smokeless tobacco. Current use of smokeless tobacco was reported by 139 (58.9%) males and 117 (49.6%) females [Table - 1]. The commonest type of smokeless tobacco used was by chewing (174, 68.5%). Current use of smokeless tobacco was higher among younger men and women [Table - 1] than in the older age group.
Alcohol consumption. Sixty-five (27.5%) males and 10 (4.2%) females had consumed alcohol in the previous 12 months [Table - 1]. Among the 65 males who consumed alcohol, 10 (15.4%) reported consuming it daily, 31 (47.7%) less than once a week and 3 (4.6%) once a month.
Consumption of fruits and vegetables. The majority of the population (410 [86.9%]) consumed fewer than four servings of fruits and vegetables per day. The frequency of consumption of these items was higher among women than among men [Table - 1]. The most commonly used cooking oil was mustard oil (385 [81.6%]), followed by sunflower oil (24 [5.1%]).
Physical activity. Insufficient physical activity was reported by only 3.4% of the respondents. The proportion reporting insufficient vigorous activity was higher among older males (44.1 %) than among younger males (31.4%); by contrast, this risk factor was less frequent among older females than among younger females (60% v. 72%; [Table - 1]).
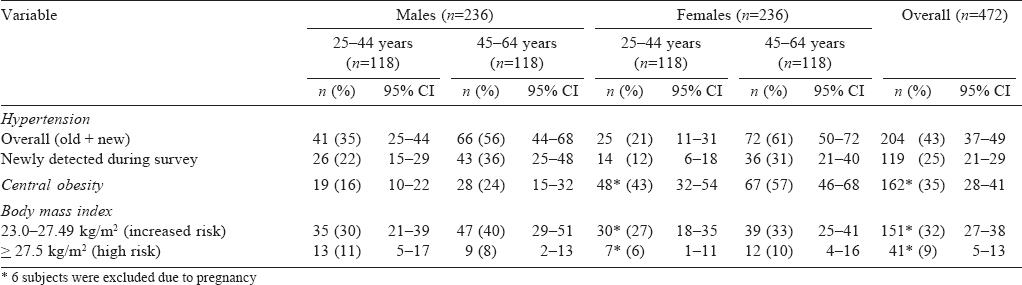
Anthropometric and blood pressure measurements
BMI above 27.49 kg/m2 was observed among 22 (9.3%) males and 19 (8.1%) females. Central obesity was identified in 47 (20%) males and 115 (48.7%) females. The prevalence of hypertension was 204/472 (43.2%), including 119 (25.2%) persons who were newly detected to have hypertension during the survey. Prevalence of hypertension was nearly double among older persons (aged 45–64 years) than among younger persons (aged 25–44 years) (58.5% v. 27.9%; [Table - 2]).
Discussion
We found tobacco use and alcohol consumption as frequent risk factors for NCDs among rural tribal adults in Mokokchung district of Nagaland. This is consistent with results of previous surveys.[6],[11]
The National Tobacco Control Programme (NTCP) has been launched in Nagaland, but has not yet been implemented in Mokokchung.[12] There is a need to intensify the tobacco control efforts in the state, in particular in rural tribal areas, to prevent young people starting to smoking and to help current smokers quit smoking.
Alcohol consumption was also frequent among those in the younger age group. Nagaland has alcohol prohibition under the Nagaland Liquor Total Prohibition (NLTP) Act, 1989.[13] Consumption of Indian-made foreign liquor (IMFL) by a large proportion of the subjects indicates poor implementation of this Act. Illegal smuggling of liquor into the state due to porous borders with the neighbouring states may also be a contributory factor. Our data emphasize the need to implement various alcohol-containment measures, including those laid down in the ‘Nagaland State Drug Abuse Prevention and Treatment Policy’.[14]
We also observed a high prevalence of inadequate intake of fruits and vegetables. Growing of these crops in Nagaland is confined mainly to small backyard gardens. Failure to grow these as commercial crops has led to poor availability of fruits and vegetables in the state.[15] Another reason for low consumption of these foods may be the sociocultural preference for eating rice and meat.
Insufficient physical activity in our study population was lower than the national estimates.[16] However, the prevalence of overweight was higher than that in the 2005–06 survey (5.7% males and 6.4% females),[17] which is disconcerting. We believe there is a need to understand the factors underlying the increase in the number of overweight people, in the context of active lifestyles followed by this rural tribal population.
There was also a high prevalence of hypertension. Hypertension has been identified as a public health priority in northeastern India. High prevalence of hypertension in this region was reported in 2001 in a study of tea-garden workers in Assam.[18] The fact that a large proportion of persons with hypertension had newly detected hypertension suggests a low awareness about hypertension in the community and lack of screening programmes.
A report from Nagaland in 2010, based on diagnoses indicated in death certificates, found that a high proportion (20%) of deaths in the state were related to cardiovascular diseases.[19] This, combined with a high prevalence of risk factors for NCDs, suggests the need for preventive measures aimed at these risk factors in the district. This may include mass media campaigns and community-based interventions to increase awareness regarding healthy eating habits, weight reduction and tobacco cessation. In addition, there is a need to strengthen primary healthcare facilities for counselling and management of hypertension, using low-cost medications, and training of paramedical and medical healthcare providers. Policy interventions to increase production and improve access to fruits and vegetable should also be helpful.
Acknowledgements
We thank the Government of Nagaland and Chief Medical Officer, Mokokchung, Nagaland for their support during the conduct of the study. We thank field investigators who did data collection and participants of the study for sparing their valuable time and resources towards completion of the survey. This study was funded by the National Institute of Epidemiology, Chennai, Tamil Nadu.
| 1. | Patel V, Chatterji S, Chisholm D, Ebrahim S, Gopalakrishna G, Mathers C, et al Chronic diseases and injuries in India. Lancet 2011;377:413-28. [Google Scholar] |
| 2. | World Health Organization. WHO STEPS Instrument (Core and Expanded). Geneva: WHO; 2015. Available at www.who.int/chp/steps/instrument/STEPS_Instrument_V3.1.pdf?ua=1 (accessed on 11 May 2015). [Google Scholar] |
| 3. | Parasuraman S, Kishor S, Singh SK, Vaidehi Y. A profile of youth in India. National Family Health Survey (NFHS-3), India, 2005–06. Mumbai:International Institute for Population Sciences; 2009. [Google Scholar] |
| 4. | National Institute of Medical Statistics, Indian Council of Medical Research (ICMR). Integrated Disease Surveillance Project (IDSP) Non-Communicable Disease Risk Factors Survey, Phase-I States of India, 2007–08. New Delhi:National Institute of Medical Statistics and Division of Non-Communicable Diseases, Indian Council of Medical Research; 2009. [Google Scholar] |
| 5. | Directotate of Census Operations Nagaland. Census of India 2011, Nagaland, District Census Handbook, Mokokchung. Kohima:Directotate of Census Operations Nagaland; 2014. [Google Scholar] |
| 6. | Ministry of Health and Family Welfare, Government of India. Global adult tobacco survey, GATS India 2009–2010. Mumbai:International Institute for Population Sciences; 2010. [Google Scholar] |
| 7. | World Health Organization. Noncommunicable diseases global monitoring framework: Indicator definitions and specifications 2014. Available at www.who.int/nmh/ncd-tools/…/GMF_Indicator_Definitions_Version_N0V2014.pdf(accessed on 6 Jan 2017). [Google Scholar] |
| 8. | Inoue S, Zimmet P, Caterson I, Chunming C, Ikeda Y, Khalid AK, et al. The Asia-Pacific perspective: Redefining obesity and its treatment. Sydney:Health Communication Australia Pty. Limited; 2000. [Google Scholar] |
| 9. | WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63. [Google Scholar] |
| 10. | Whitworth JA, World Health Organization (WHO)/International Society of Hypertension (ISH) Writing Group. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hyperten 2003;21:1983-92. [Google Scholar] |
| 11. | Ministry of Health and Family Welfare, Government of India. District level household and facility survey-4, District fact sheet Mokokchung (2012–13). Mumbai: International Institute for Population Sciences; 2012-13. [Google Scholar] |
| 12. | Government of Nagaland. National Tobacco Control Programme (NTCP). Nagaland, Kohima:Department of Health and Family Welfare, Nagaland. Available at http://nagahealth.nic.in/programmes-NRHIM-NTCP.htm (accessed on 10 May 2015). [Google Scholar] |
| 13. | Government of Nagaland. State Judiciary, List of Acts. Available at http://nagaland.nic.in/functionaries/department/judiciary/list-acts.htm (accessed on 10 May 2015). [Google Scholar] |
| 14. | Drug, liquor smuggling on the rise. Nagaland Post Jun 27, 2016. Available at http://issuu.com/nagalandpost90/docs/june_27_2016/2 (accessed on 6 Jan 2017). [Google Scholar] |
| 15. | Karmakar KG, Banerjee GD. Horticultural boom in Nagaland. Mumbai:National Bank for Agriculture and Rural Development (NABARD); 2014. Available at www.nabard.org/pdf/Horticultural Boomin Nagaland.pdf (accessed on 30 May 2015). [Google Scholar] |
| 16. | World Health Organization. Global status report on noncommunicable diseases 2014. Geneva:WHO; 2014. [Google Scholar] |
| 17. | International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), India, 2005–06: Nagaland. Mumbai:International Institute for Population Sciences (IIPS); 2009. [Google Scholar] |
| 18. | Hazarika N, Biswas D, Narain K, Kalita H, Mahanta J. Hypertension and its risk factors in tea garden workers of Assam. Natl Med J India 2001;15:63-8. [Google Scholar] |
| 19. | Offce of Registrar General India. Report on Medical Certification of Cause of Death 2010. New Delhi:Ministry of Home Affairs, Government of India; 2014. Available at www.censusindia.gov.in/2011-Documents/mccd_Report1/MCCD-Report-2010.pdf (accessed on 30 May 2015) [Google Scholar] |
Fulltext Views
2,308
PDF downloads
10,277




